How to Make a Nervine Tea Blend for Stress
Contents
- 1 The four herbs in this blend—and what the research says
- 2 The evidence perspective
- 3 Your stress-soothing nervine tea blend
- 4 How to brew it (step-by-step)
- 5 How often to drink it
- 6 Storage, freshness, and safety tips
- 7 Important cautions (please read before you brew)
- 8 Taste tweaks and gentle add-ins
- 9 Troubleshooting: what if you don’t feel calmer?
- 10 Frequently asked questions
- 11 When to get help
- 12 References

Young adults consistently report high stress—and many want calming options they can make at home. In APA’s Stress in America reporting, Gen Z and Millennials have repeatedly described higher stress levels and more stress-related symptoms than older cohorts, with Gen Z’s average stress higher than the overall average in recent years.
Nervine tea herbs are plants traditionally used to ease mild tension, support relaxation, and help with sleep hygiene; examples include chamomile, lemon balm, passionflower, and linden, each of which has European Medicines Agency (EMA) monographs describing traditional use and dosing for infusions (“herbal teas”).
Bottom line: A thoughtfully designed, safety-first tea can be one small, soothing part of a broader stress-care routine. Evidence supports mild calming effects for several nervine herbs, though these teas are not treatments for clinical anxiety.
The four herbs in this blend—and what the research says
Below are the herbs I chose for a beginner-friendly, great-tasting blend. For each, you’ll see a short evidence snapshot plus the EMA’s tea dosing guidance (where available).
1) Chamomile (Matricaria recutita) — classic calm

- Evidence snapshot: A randomized, double-blind, placebo-controlled trial found chamomile extract produced modest anxiolytic effects in patients with generalized anxiety disorder (GAD). (Amsterdam et al., 2009) Follow-up work also suggests benefits for anxiety symptom reduction, though more and larger trials are needed. (Mao et al., 2016)
- Safety notes: Allergic reactions can occur—especially in people allergic to ragweed and related Asteraceae plants. (NCCIH—Chamomile) There is a published case report of a warfarin–chamomile interaction leading to bleeding; anyone on blood thinners should discuss chamomile with a clinician. (CMAJ case report)
- Tea dosing (EMA): 1.5–4 g dried flowers infused in 150 mL boiling water per dose.
2) Lemon balm (Melissa officinalis) — bright, lemony, mood-steadying

- Evidence snapshot: Small placebo-controlled studies and reviews show short-term reductions in state anxiety and improvements in calmness and mood after lemon balm preparations; heterogeneity is high and more robust trials are needed. (Scholey & co-authors, 2014; Ghazizadeh et al., 2021; Mathews et al., 2024)
- Safety notes: EMA notes in-vitro/animal data suggesting lemon balm extracts may inhibit TSH activity (thyroid-related), with unknown clinical relevance—so people with thyroid disease or on thyroid medication should seek medical advice. (EMA monograph; EMA assessment report)
- Tea dosing (EMA): 1.5–4.5 g dried leaf infused in 150 mL boiling water per dose. (EMA lemon balm monograph)
3) Passionflower (Passiflora incarnata) — gentle, slightly sedating

- Evidence snapshot: A small double-blind trial in GAD found passionflower extract had anxiolytic effects comparable to oxazepam over 4 weeks (pilot data; methods limitations). (Akhondzadeh et al., 2001) The EMA review concludes evidence is insufficient for well-established use but supports traditional use for relief of mild stress and to aid sleep. (EMA assessment report)
- Safety notes: May cause drowsiness; avoid driving/operating machinery if affected and avoid combining with other sedatives. Not recommended in pregnancy or lactation due to insufficient data. (EMA assessment report—safety; NCCIH—Passionflower)
- Tea dosing (EMA tradition): EMA recognizes comminuted herb infusions within traditional-use products; daily crude herb intake in reports typically ~4–8 g/day, divided. (EMA assessment report)
4) Linden (Tilia spp., “lime blossom”) — floral, soothing

- Evidence snapshot: Linden flowers are traditionally used as a calming beverage; clinical data are limited, and EMA categorizes it under traditional use for relief of mild symptoms of stress and to aid sleep.
- Tea dosing (EMA): 1.5 g dried flowers infused in 150 mL boiling water per single dose (frequency per product monograph/traditional preparations).
The evidence perspective
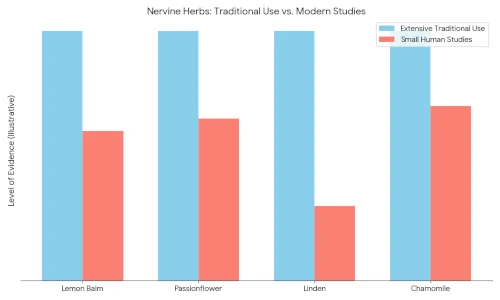
- These herbs have encouraging though mostly small human studies and strong traditional use records for easing mild tension or supporting sleep; they are not substitutes for evidence-based treatment of anxiety disorders. (Amsterdam 2009; Akhondzadeh 2001; EMA passionflower assessment; AAFP clinical review)
- First-line care for anxiety disorders includes psychotherapy (especially CBT) and/or medications such as SSRIs, based on guidelines. (APA patient education; NICE guideline overview)
Your stress-soothing nervine tea blend
This recipe uses weight for accuracy and to stay within EMA tea posology when prepared by the cup. If you don’t have a scale, see the spoon conversions below.
Blend ratio (by weight)
- 2 parts lemon balm (aromatic leaf)
- 2 parts chamomile (flower heads)
- 1 part passionflower (aerial parts)
- 1 part linden (flowers with bracts)
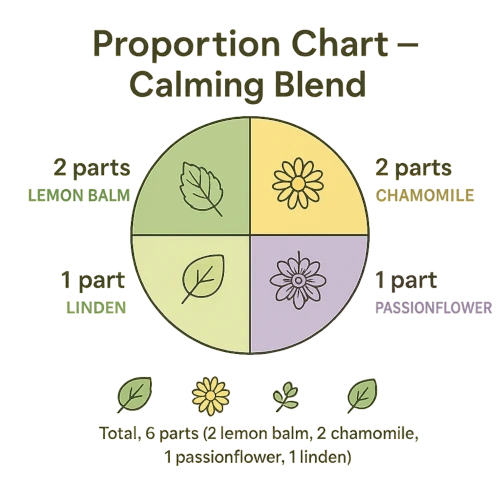
For a small jar (~80 g total), that’s 20 g lemon balm + 20 g chamomile + 10 g passionflower + 10 g linden (repeat the pattern until you reach your target weight). This proportional approach keeps each herb near the lower end of its per-cup traditional tea dose when brewed as directed below. (EMA lemon balm monograph; EMA passionflower assessment)
Spoon conversions (approximate)
If you’re measuring by volume, a common herb-kitchen conversion handout equates 1 g dried herb ≈ 1.5 teaspoons (this varies by cut/leaf size; weighing is best).
How to brew it (step-by-step)
What you’ll need
- Your nervine blend
- Kettle and heatproof mug or teapot
- Fine mesh strainer or French press
- Lid/saucer to cover while steeping
- Timer
Per-cup method (one serving)

Measure the tea: Add ~2.5 g of the blend to your mug/teapot (≈ ~4 tsp loose herb using the 1 g ≈ 1.5 tsp estimate). This yields a total herb amount that keeps each plant within the typical 150 mL infusion dose described in EMA monographs.

Add water: Pour ~150–200 mL just-boiled water over the herbs. EMA tea posologies specify 150 mL boiling water per dose for these herbs.

Cover and steep: Cover the mug and steep ~10 minutes. Covering helps keep volatile aromatics from evaporating into the steam.
Strain and sip: Strain and let it cool briefly; avoid drinking beverages hotter than ~65 °C (149 °F) because very hot drinks have been classified by IARC as probably carcinogenic to the esophagus.
Batch option

- Add ~10 g of the blend to ~750–800 mL just-boiled water in a teapot, cover, and steep 10–15 minutes; strain into a thermos to keep warm. This scales the per-cup dosing above. (EMA monographs)
How often to drink it

- For short-term use, many traditional tea monographs specify 1 dose, up to several times daily. A practical starting point is 1–2 cups/day, adjusting based on how you feel and your clinician’s advice—especially to avoid excess drowsiness from passionflower.
- If your symptoms persist beyond about 2 weeks or are interfering with daily life, seek professional care; clinical guidelines favor CBT and/or antidepressants (SSRIs/SNRIs) for anxiety disorders.
Storage, freshness, and safety tips

- Store dried herbs airtight in a cool, dark, dry place; university extension guidance notes dried herbs are best within ~1 year under good storage. (Oregon State University Extension PDF; South Dakota State University Extension)
- Label your jar with the herb names and date. This supports safer use, especially if you share a kitchen. (General safety guidance: NCCIH—Safety hub)
- Cover while steeping to retain aromatics; covering is standard advice from culinary-nutrition and herbal infusion references.
- Let very hot tea cool; beverages >65 °C are in IARC’s Group 2A (“probably carcinogenic”) because of thermal injury risk to the esophagus—not because of the tea itself. (IARC press release; IARC Q&A)
Important cautions (please read before you brew)
- Allergies: Chamomile can trigger reactions in people allergic to ragweed and related Asteraceae plants (chrysanthemums, marigolds, daisies). (NCCIH—Chamomile)
- Blood thinners: A serious warfarin–chamomile interaction has been reported; if you take anticoagulants or antiplatelets, talk with your clinician first. (CMAJ case report)
- Sedation & driving: Passionflower can cause drowsiness; avoid driving or operating machinery if you feel sedated, and avoid combining with other sedatives unless your clinician says it’s okay. (EMA passionflower assessment—driving caution)
- Thyroid considerations: Lemon balm has in-vitro/animal data suggesting TSH inhibition, with uncertain clinical relevance; use caution and consult a clinician if you have thyroid disease or take thyroid medication. (EMA lemon balm monograph; EMA assessment report)
- Pregnancy & lactation: Safety data are limited for several herbs in pregnancy/lactation; avoid passionflower and use caution with chamomile (observational signals are mixed) unless specifically cleared by your prenatal clinician. (NCCIH—Passionflower; NCCIH—Chamomile; Review of herbal tea use in pregnancy)
- Quality matters: Herbal products are regulated differently from drugs in the U.S.; product variability exists. Choose reputable suppliers and follow labeling. (NCCIH—Chamomile: regulatory note)
Taste tweaks and gentle add-ins

- Citrus twist: A strip of lemon peel brightens chamomile/lemon balm (no specific health claim—just flavor).
- Aroma boost: A small pinch of dried lavender flowers can add perfume; note that most clinical anxiety data center on standardized oral lavender oil (Silexan) rather than lavender tea.
- Evening routine pairing: Combine tea time with CBT-informed sleep hygiene (consistent schedule, lights down) when worry peaks; CBT is first-line for anxiety disorders.
Troubleshooting: what if you don’t feel calmer?

- Adjust steep time or dose—gently. Keep within the EMA per-cup ranges above and try 10–15 minutes covered steeping for a fuller infusion.
- Try timing: Many people prefer late afternoon or evening for passionflower-containing blends to avoid daytime drowsiness.
- Look at the big picture: Persistent anxiety, sleep disruption, or intrusive worry deserve evidence-based care—CBT and/or medications per guidelines—alongside any lifestyle strategies.
Frequently asked questions
Can I swap in or add other calming herbs?
Yes—common additions include peppermint (flavor; not a sedative) or oatstraw (traditional tonic); check a reputable monograph for dosing and contraindications before swapping. (General safety hub: NCCIH—Safety; monograph examples: EMA peppermint monograph)
Is lavender tea the same as lavender oil capsules?
No. Most anxiety RCTs involve standardized oral lavender oil (Silexan), not tea; effects can’t be assumed equivalent. (Meta-analysis)
How long do dried herbs stay good?
Stored airtight in a cool, dark cupboard, most dried culinary herbs are best within ~1 year; potency and aroma fade faster if exposed to air/light/heat. (OSU Extension PDF; SDSU Extension)
Why cover the mug?
It helps retain volatile aromatics (what you smell in the steam)—one reason professional dietitians and herbal educators advise covering during steeping.
Is “tea too hot” a real issue?
Yes. Very hot drinks (>65 °C / 149 °F) are an IARC Group 2A risk due to thermal injury to the esophagus. Let your tea cool a bit before sipping. (IARC press release)
When to get help
If worry, panic, or insomnia is persistent or worsening, or you’re losing work/school/social functioning, connect with a licensed professional. CBT and medications like SSRIs are proven options and can be combined with supportive habits (including tea time). (APA patient guidance; AAFP review; NICE guideline overview)
Brew the blend, notice how your body responds, and—if stress is taking over—book an appointment with a counselor, therapist, or your primary care clinician this week. Bring a list of your symptoms, what you’ve tried (including this tea), and any medications/supplements you use so you can choose a plan grounded in evidence and tailored to you. (APA patient guidance)
HEALTH DISCLAIMER: The information on this website is for educational uses only and is not a substitute for professional medical advice. Always consult an authorized healthcare provider for any health concerns before using any herbal or natural remedy. We do not establish, treat, cure, or prevent any disease. Reliance on any material from this website is solely at your own risk. We are not responsible for any adverse effects resulting from the use of information or products mentioned on this website.
References
- APA. Gen Z & Millennials stress—overview: APA 2023 summary
- APA. Gen Z stress—full 2018 report: PDF
- APA. Gen Z stressed—news release: Webpage
- AAFP. GAD & panic: treatments (CBT/SSRIs): Clinical review
- APA. Anxiety disorders: patient education: Webpage
- NICE CG113. GAD/panic in adults: Guideline overview
- EMA. Lemon balm (Melissa officinalis) monograph—tea dosing: PDF
- EMA. Lemon balm assessment—thyroid note: PDF
- EMA. Passionflower (Passiflora) assessment—sedation/driving caution; traditional use: PDF
- Amsterdam JD et al., 2009. Chamomile RCT in GAD: PubMed
- Mao JJ et al., 2016. Long-term chamomile: Abstract
- Akhondzadeh S et al., 2001. Passionflower vs oxazepam (pilot RCT): PubMed
- Scholey A et al., 2014. Lemon balm & mood/calmness: Open-access review
- Ghazizadeh J et al., 2021. Lemon balm—systematic review: PubMed
- Mathews IM et al., 2024. Lemon balm—clinical efficacy & tolerability: Open-access review
- Kasper M et al., 2023. Lavender oil (Silexan) meta-analysis: Open-access
- NCCIH. Chamomile safety (allergies/regulation): Webpage
- CMAJ/Segal R, 2006. Warfarin–chamomile interaction case report: Open-access
- NCCIH. Passionflower safety: Webpage
- IARC/WHO, 2016. Very hot beverages (>65 °C) risk: Press release and Q&A
- Oregon State University Extension. Storing dried herbs: PDF
- South Dakota State University Extension. Herb storage & use: Webpage
Last update on 2025-12-20 / Affiliate links / Images from Amazon Product Advertising API






